JAWBONE CAVITATIONS
These hidden, mostly asymptomatic lesions cause inflammation & negatively affects the health of millions of people.
Introduction
In the field of dentistry and oral health, understanding various dental conditions and their implications for systemic health is crucial for providing optimal care to patients. One such condition that has gained attention in recent years is "jawbone cavitations." The International Academy of Oral Medicine and Toxicology (IAOMT) published a position paper in 2014 shedding light on this topic.
Jawbone cavitations, often referred to as "cavitations" or "ischemic osteonecrosis," are areas of dead or necrotic bone in the jawbone. They are typically found in the jawbone where a tooth extraction, especially wisdom teeth, or oral surgery has taken place. These areas may not heal properly and can become a breeding ground for bacteria and toxins, having great potential for contributing to chronic health issues.
Recently, the IAOMT has released an updated position paper on Human Jawbone Cavitations, providing a thorough analysis and insights into this complex medical-dental condition. The paper is a collaborative effort of renowned experts in the field, aiming to shed light on the diagnosis, risk factors, systemic implications, and treatment modalities associated with jawbone cavitations.
Drawing upon detailed histological observations, the IAOMT has recommended a name that aligns more closely with the scientific and medical aspects of the condition known as Jawbone Osteonecrosis. This proposed name is "Chronic Ischemic Medullary Disease of the Jawbone" or CIMDJ. By adopting this terminology, we aim to provide a more precise and accurate representation of the underlying pathological processes and characteristics associated with this condition.
In this article, we explore the history, diagnosis, risk factors, systemic and clinical implications, treatment modalities, and conclusions related to jawbone osteonecrosis. We also delve into the evolving considerations for diagnostic purposes, such as thermography and acupuncture meridian assessment. Additionally, we will highlight alternative treatment strategies and provide an overview of the IAOMT survey results on the resolution of systemic symptoms following cavitation surgery.
History
Throughout its history, what we are referring to as CIMDJ has been referred to by a multitude of names and acronyms that are listed in Table 1 and are briefly discussed below.
Jawbone cavitations have been diagnosed, treated, and researched since the 1860s. Over the years, various names and acronyms have been used to describe this condition, including neuralgia-inducing cavitational osteonecrosis (NICO) and chronic fibrosing osteomyelitis (CFO).
Research on jawbone cavitations seemed to come to a halt until the 1970s when others began researching the topic and publishing information regarding it in modern oral pathology textbooks. Since 2010, Dr. Johann Lechner, the most widely published author and researcher on jawbone cavitational lesions, and others have been researching the relationship of these lesions to cytokine production, especially the inflammatory cytokine RANTES (also known as CCL5).
Diagnosis
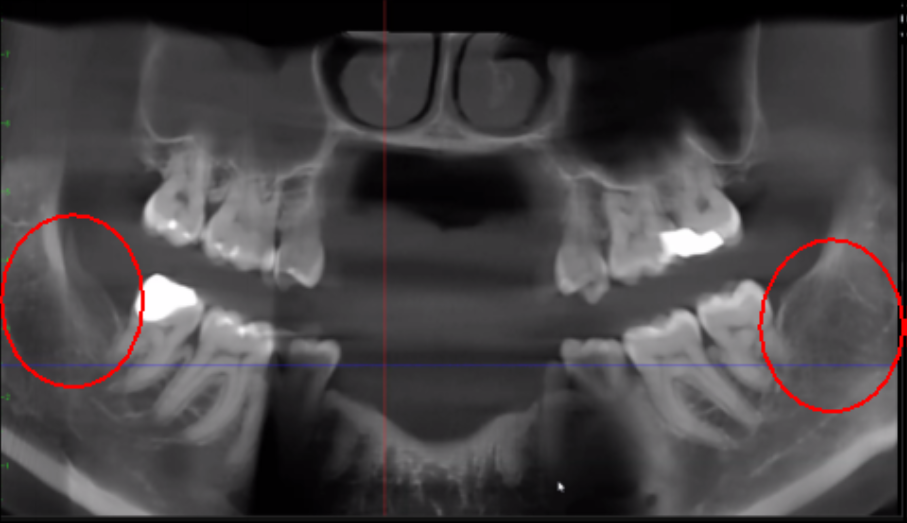
The use of Cone-Beam Computed Tomography (CBCT) radiographs (CAT scan) has become increasingly common in diagnosing jawbone cavitations. CBCT radiographs have contributed to the identification of these cavitations, which were previously overlooked. These cavitations are often not detected on standard 2D radiographic films. CBCT provides a 3D view of the lesion, allowing for better identification of the size, extent, and contents of the cavity. Recently developed software that is specifically integrated with different types of CBCT devices allows for a standardized assessment of bone density which helps the dentist verify the presence of any cavitations in the jawbone.
Ultrasound devices, such as CaviTAU™®, have also been developed for detecting low bone density areas suggestive of jawbone cavitations. Developed in Germany, this device is currently unavailable in the U.S. but is under review by the U.S. Food and Drug Administration. Biomarkers, such as cytokines, have been investigated as diagnostic tools for jawbone osteonecrosis.
Because of the inflammatory nature of jawbone cavitations, researchers have investigated the possible relationship between select cytokines and the disease. Additionally, the use of ultrasound, biomarkers, and histological examination are discussed as evolving considerations for diagnostic purposes.
Risk Factors
The development of jawbone cavitations can be attributed to various risk factors, including external influences such as environmental factors and internal influences such as poor immune function. Genetic predisposition may also play a role in the development of jawbone osteonecrosis. Hypercoagulation, or excessive production of blood clots, has been identified as a common risk factor for jawbone cavitations. An important consideration when diagnosing and treating jawbone cavitations is whether the individual is taking antidepressants, specifically selective serotonin reuptake inhibitors (SSRIs). SSRIs have been associated with reduced bone mass density and increased fracture rates. The SSRI Fluoxetine (Prozac—which contains fluoride) directly inhibits osteoblast differentiation and mineralization.
Systemic and Clinical Implications
Jawbone cavitations have been associated with a wide range of systemic and clinical implications. The most unique and groundbreaking realization that have come to light since the IAOMT 2014 position paper is the improvement or resolution of seemingly unrelated chronic inflammatory conditions following cavitation treatment. Whether systemic illnesses are of an autoimmune nature or inflammation occurring otherwise, significant improvements have been reported. Examples of conditions that have remitted following treatment include chronic fatigue syndrome, irritable bowel syndrome, brain fog, arthritis, and localized jaw pain, among others. The presence of cytokines generated in the necrotic lesions of cavitations can contribute to the development and progression of chronic inflammatory diseases. Research has shown that the treatment of cavitations can lead to improvements in quality of life and a reduction in symptoms associated with systemic illnesses.
Treatment Modalities
Surgical therapy is often recommended for the treatment of jawbone cavitations. This involves excising the affected non-vital bone, thoroughly cleaning out the lesion, and promoting the regrowth of normal, vital bone. Platelet-rich fibrin (PRF) grafts and other adjunctive therapies may be used to enhance healing.
Preconditioning may also contribute to successful treatment outcomes. This involves creating a tissue environment conducive to healing by supplying the body with adequate levels of appropriate nutrients that improve the biological terrain by optimizing homeostasis in the body. Ideally, the reduction of any toxic load on the body such as fluoride and/or mercury from dental amalgam fillings should be completed before treatment of jawbone cavitations. As mentioned above, if the individual is taking selective serotonin reuptake inhibitors (SSRIs) such as Fluoxetine (Prozac—which contains fluoride) bone health can be altered.
Alternative treatment strategies, such as homeopathy, electrical stimulation, red light therapy such as photobiomodulation and laser, medical grade oxygen/ozone, hyperbaric oxygen, anticoagulation modalities, Sanum remedies, nutrition and nutraceuticals, infra-red sauna, intravenous ozone therapy, energy treatments, and others are also being explored but require further research to determine their efficacy.
IAOMT Survey Results
The first survey was conducted to learn more about what types of conditions resolve and how close to surgery remission occurs (see Appendix 1 in full paper). Respondents rated the level of improvement (mild, moderate or significant) and noted whether improvement occurred rapidly (0-2 months) or took longer (> 2 months). Localized jaw pain, brain fog, arthritis, chronic fatigue syndrome and other autoimmune disorders were the most common conditions reported and most symptoms remitted in less than two months. Additionally, respondents were queried on whether they typically performed surgery on individual sites (almost half), multiple unilateral sites (less than a quarter), or all sites in one surgery (about one/third).
The second survey was to gather information regarding what trends and treatments are developing toward a ‘standard of care’ (see Appendix 2 in full paper). To briefly summarize the results, most respondents are offered surgical treatment, which involves soft tissue reflection, surgical access of the cavitation site, and various methods of physically ‘cleaning out’ and disinfecting the affected site. Most respondents do not biopsy the lesions stating a variety of reasons including cost, inability to obtain viable tissue samples, difficulty in finding a pathology lab, or certainty of the status of the disease. After cleaning, most respondents use ozone water/gas to disinfect and promote healing. PRF (platelet-rich fibrin) and PRP (platelet-rich plasma) are also commonly used. A wide range of medicaments, nutraceuticals, and/or blood products are used to promote healing of the lesion prior to closing the soft tissue incision. Most respondents do not use antibiotics pre-operatively, during surgery or post-operatively. Many respondents use Vitamins C and/or utilize low level laser therapy post operatively for healing purposes.
Conclusions
Jawbone osteonecrosis, or chronic ischemic medullary disease of the jawbone (CIMDJ), is a complex condition that requires thorough diagnosis and treatment. CBCT and other imaging techniques have greatly improved the identification and understanding of jawbone cavitations. The link between jawbone cavitations and systemic illnesses highlights the importance of recognizing and treating these lesions. Surgical therapy remains the favored treatment modality, but alternative approaches are being explored. Further research is needed to establish standardized protocols and determine the long-term outcomes of different treatment strategies.
For more detailed information about Chronic Ischemic Medullary Disease of the jawbone please read our full position paper entitled, “IAOMT Position Paper on Human Jawbone Cavitations”.







Thank you, this is an insidious crisis in the U.S. Affected former patients are extraordinarily underserved by almost all practitioners here. Many don't even realize our healthcare system fails to help and oftentimes harms the chronically diseased. This "care" is even exponentially worse for those with obscure diseases like cavitations. I seem to have no legal recourse for the extreme, systemic damage that my past cavitations had. I believe the DOE (education) is primarily to blame for not better ensuring cavitations do not occur nor become infected. Biological dentists do a much better job in general with these precautions. Cavitations have been known about for over a century. There's no excuse for the pathology not to be accepted as existent by all dental regulators and overseers. The dentist that failed with my extractions many yrs ago still abided by most if not all of his requirements for care. I still have pulpitis in most if not all of my teeth from the metastatic cavitational infections. I may literally have to have all my teeth pulled. Regenerative endodontics is developing in research but I can't find a dentist that offers this for adults near NY. Any help here would be GREATLY appreciated.
Could you please provide specific "cytokine" bloodwork that you speak to in the article?